TRoMbone is launched!
TRoMbone is launched! The UK feasibility randomised trial Testing radical prostatectomy in men with prostate cancer and oligoMetastases to the bone has opened at Oxford University Hospitals (PI Freddie Hamdy), University College London Hospitals (PI John Kelly) and Royal Surrey County Hospital (PI Chris Eden). Men <75 with newly-diagnosed prostate cancer and 1-3 skeletal lesions on any standard-of-care imaging (CT, bone scan, MRI, or PET) who are fit for surgery and deemed to be technically operable are eligible. Emerging but lower-quality data suggests a role for treatment of the primary tumour in men with oligo-metastatic prostate cancer and this UK study will investigate this question with level 1 evidence.
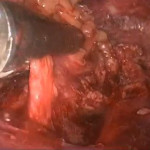
Participants will be randomly allocated to standard-of-care treatment (hormones +/- chemotherapy) versus standard-of-care treatment plus surgery to remove the prostate and draining lymph nodes (radical prostatectomy plus extended pelvic lymphadenectomy). A qualitative recruitment investigation to optimise accrual will be conducted by the University of Bristol (Caroline Wilson) and biologic samples will be collected, processed and stored in a repository at the Institute of Cancer Research (Gerhardt Attard).
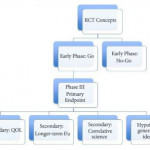
We will assess technical feasibility, safety and complications of surgery in oligo-metastatic prostate cancer, and examine ways to improve recruitment in this pilot study. TRoMbone is managed by the Surgical Intervention Trials Unit at the University of Oxford and funded by the Prostate Cancer Foundation and The Urology Foundation.
We need to recruit 50 men over a 12-month period, and are seeking referrals from other centres to increase accrual. Centres that demonstrate ability to refer eligible patients will be able to take part in the main trial if we can demonstrate feasibility in this phase and get funding for the larger study.
So please look out for these patients and send them to me at UCLH, Freddie in Oxford, or Chris in Guildford. One of the three of us will do the surgery if they get randomised to it, but of course you’re welcome to come with the patients. If you have any queries please contact me, the study CI (P. Sooriakumaran (PS); prasanna.sooriakumaran@nds.ox.ac.uk) or the study co-ordinator (Neelam Hassanali; trombone@nds.ox.ac.uk). You can start them on androgen deprivation and ‘stop the clock’ before you refer them to us. The extra burden of participating in this study is minimal. They will require one visit for consent, and one follow-up visit at 3 months after randomisation. The surgical group will also have two other visits for their surgery and catheter removal. The rest of the follow-up can be done back at your referring centre or with us, whatever you and the patient prefer. If it’s your standard policy to give them chemotherapy or metastasis-directed therapy with SBRT then you can still do that as part of the study.
With your help we can demonstrate that this study is feasible in the UK and we can lead the way in the surgical management of oligo-metastatic prostate cancer.
P. Sooriakumaran [social type=”facebook” opacity=”dark’ label=’PLACE_LINK_HERE[/social]
BMedSci(Hons) BMBS(Hons) PhD PGCMedLaw ADCClinInv FRCS(Urol) FEBU USLME
Consultant Urological Surgeon, UCL Hospitals NHS Foundation Trust & Honorary Clinical Senior Researcher, University of Oxford


Congrats P.S. and good luck with your trial.
This question will have significant study with level 1 evidence in the near future.
Our trial at MD Anderson Cancer Center in Houston (clinicaltrials.gov NCT01751438) is partnered with UC San Francisco, Vancouver Prostate Center, and Fox Chase Cancer Center. It treats men with metastatic prostate cancer (no definition of oligo) with 6 months ADT and then randomizes to local therapy (surgery or XRT) versus best systemic therapy only. To be enrolled they have to respond to ADT in the first 6 months.
The current update: target accrual of 120, starting March 2013, 90 randomized, 15 pending their 6 mo ADT, and 15 left to accrue–hopefully done by July 2017 and progression free initial read out summer 2018. This design is planned for phase III SWOG study as well.
As you can see by trial design, there are differences in including metastatic disease that has a reasonable androgen deprivation response, versus defining subsets of oligometastatic disease. Otherwise, the concepts are similar and hopefully will make a difference in patient care.
Thx John. Yes, the Chapin trial complements TRoMbone nicely. Results are eagerly awaited.
Exciting to see TRoMbone launced PS. Thank you for the helpful blog setting things out nicely. As someone who has spent a year in Melbourne with some of the most knowledgeable proponents of PSMA imaging (Perera et al & Lawrentschuk, Eur Urol 2016) and working alongside a great lab team who demonstrated so effectively the importance of clonal dissemintation and re-seeding in advanced disease (Hong et al & Hovans & Corcoran, Nature Comms 2015) I personally feel that we’re on the verge of a new paradigm in Prostate Cancer management (Sathianathan et al & Lamb, Future Oncoogy 2017).
My hope is that the TRoMbone study (alongside Chapin and others) will provide the evidence that we need to embark on a new, anti-nihilistic approach to managing metastatic prostate cancer. It makes sense that the source of aggressive cancer clones, the in-situ prostate, is removed when safe to do so, much in the manner that a seeded Dandelion is still worth removing to prevent future dissemination.
Having just started as your replacement at Oxford I look forward to managing these men!