Video: TRUS-Guided RB Prostate Cancer Detection – Reasons for Targeted Biopsy Failure
Prostate cancer detection on transrectal ultrasonography-guided random biopsy despite negative real-time magnetic resonance imaging/ultrasonography fusion-guided targeted biopsy: reasons for targeted biopsy failure
Objective
To examine the value of additional transrectal ultrasonography (TRUS)-guided random biopsy (RB) in patients with negative magnetic resonance imaging (MRI)/ultrasonography (US) fusion-guided targeted biopsy (TB) and to identify possible reasons for TB failure.
Patients and Methods
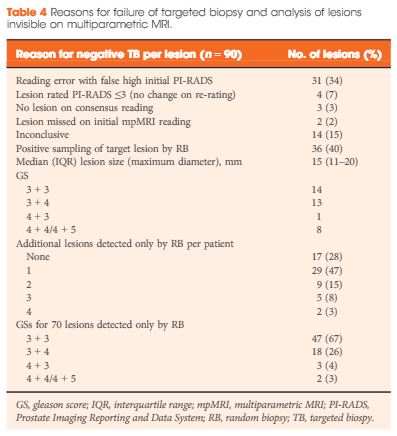
We conducted a subgroup analysis of 61 men with prostate cancer (PCa) detected by 10-core RB but with a negative TB, from a cohort of 408 men with suspicious multiparametric magnetic resonance imaging (mpMRI) between January 2012 and January 2015. A consensus re-reading of mpMRI results (using Prostate Imaging Reporting and Data System [PI-RADS] versions 1 and 2) for each suspicious lesion was performed, with the image reader blinded to the biopsy results, followed by an unblinded anatomical correlation of the lesion on mpMRI to the biopsy result. The potential reasons for TB failure were estimated for each lesion. We defined clinically significant PCa according to the Epstein criteria and stratified patients into risk groups according to the European Association of Urology guidelines.
Results
Our analysis showed that RB detected significant PCa in 64% of patients (39/61) and intermediate-/high-risk PCa in 57% of patients (35/61). The initial mpMRI reading identified 90 suspicious lesions in the cohort. Blinded consensus re-reading of the mpMRI led to PI-RADS score downgrading of 45 lesions (50%) and upgrading of 13 lesions (14%); thus, negative TB could be explained by falsely high initial PI-RADS scores for 32 lesions (34%) and sampling of the target lesion by RB in the corresponding anatomical site for 36 out of 90 lesions (40%) in 35 of 61 patients (57%). Sampling of the target lesion by RB was most likely for lesions with PI-RADS scores of 4/5 and Gleason scores (GS) of ≥7. A total of 70 PCa lesions (67% with GS 6) in 44 patients (72%) were sampled from prostatic sites with no abnormalities on mpMRI.
Conclusion
In cases of TB failure, RB still detected a high rate of significant PCa. The main reason for a negative TB was a TB error, compensated for by positive sampling of the target lesion by the additional RB, and the second reason for TB failure was a falsely high initial PI-RADS score. The challenges that arise for both MRI diagnostics and prostate lesion sampling are evident in our data and support the integration of RB into the TB workflow.



Asbach and Cash’s video is good fun. But they have a serious message that the diagnostic pathway they describe is not very good at all. The report that 61 of their men (out of 408) had to go through the worry of no less than 3 procedures (mpMRI, TB and then 10 core RB) to get their result. In nearly 25% of these cases (14 men), the patients are left with the worry that the discrepancy between their suspicious MRI and their negative biopsy result could not be explained, and this leaves them in the unsatisfactory position that they may be facing a fourth procedure! It is not very nice to have to have up to four procedures.
MRI is very popular and it has been the new and coming thing since the brilliant work of Jelle Barentsz and other popularised 3T mpMRI, and explained its many benefits. Urologists today often signal to each other that they are up to date by their recommendations of it.
However, the problem is that, as a methodology, mpMRI and biopsy (whether TB, TP or RB) is sufficiently far from being completely reliable that one must doubt that it is the real solution to diagnosis.
If 14 out of 408 cases are left in doubt, that’s 3.5%, which I say is a lot.
I say the profession has a duty to promote the best current method for accurate clear and certain diagnosis with the least intrusion into patients’ lives and that a solution is staring the profession in the face, but the profession is not recognising it. Dogs detect CaP quite accurate, easily, and unintrusively. There are many papers on this now, but if I take a recent representative one from the Journal of Urology at random, https://www.jurology.com/article/S0022-5347(14)04573-X/abstract, the result for two dogs was described as follows:
“For dog 1 sensitivity was 100% (95% CI 99.0–100.0) and specificity was 98.7% (95% CI 97.3–99.5). For dog 2 sensitivity was 98.6% (95% CI 96.8–99.6) and specificity was 97.6% (95% CI 95.9–98.7). When considering only men older than 45 years in the control group, dog 1 achieved 100% sensitivity and 98% specificity (95% CI 96–99.2), and dog 2 achieved 98.6% sensitivity (95% CI 96.8–99.6) and 96.4% specificity (95% CI 93.9–98.1). Analysis of false-positive cases revealed no consistent pattern in participant demographics or tumor characteristics.”
Compare that to Asbach and Cash!
While it is great to research the profession’s stock in trade of mpMRI and biopsy, is it not already plain that the deficiencies of 3T MRI and biopsy are methodological limitations imposed by the techniques used and nice guys working together are not going to overcome those. I am sure there can be improvements: one example may be better higher powered MRI techniques may come in future.
However, since there is a huge gap between the accuracy of the profession’s method and the results that dogs achieve, I do ask: if we already have a method that is more accurate and less intrusive than the one the profession is using, and is one proven by many applications (police, mountain rescue, drugs etc) and is based on something Nature has developed in these animals over millions of years, why is the profession still reluctant to back research and development into that a diagnostic pathway when it is plainly better and more promising than anything the excellent Asbach and Cash are describing.