Rocktober – Keep on rocking #urojc
We celebrated the two-year anniversary of the international urology journal club this month (@iurojc) with record participation. There were over 500 tweets in the 48 hour discussion of this month’s article, published in New England Journal of Medicine on September 18, 2014, Ultrasound versus Computed Tomography for Suspected Nephrolithiasis. It was a true multidisciplinary discussion with nephrologists, EM docs, and study author, radiologist Rebecca Smith-Bindman tweeting.
This was a multi-institutional prospective randomized control study evaluating bedside and radiology ultrasonography versus CT as the first test performed for patients presenting to the ED with flank or abdominal pain. Patients who initially underwent ultrasound could also receive a CT if the provider felt necessary based on clinical presentation and ultrasound findings. In terms of the primary endpoints, authors found no significant difference across the three groups in high-risk diagnoses with complications related to missed or delayed diagnoses. There was significantly less 6-month cumulative radiation exposure in patients assigned to the ultrasonography groups compared to those assigned to CT. Conclusions of this study in the form of a tweet: Get US first #noharmdone #lessradiation.
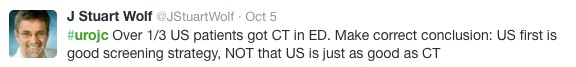
Conversation first focused on clarifying the main conclusions of this article. Notably, ED physicians were the focus of this study, who care whether the patient will be admitted or sent home. Information about size, location, etc of stones was omitted from the study since the goal was not definitive stone treatment.
Some of the limitations of the study were brought up early on. First of all, obese patients were excluded (men >129 kg and women >113 kg).
Additionally, the definition of being diagnosed with a stone only applied to individuals who reported passing a stone or having a stone surgically removed.
Much of the conversation focused on how this approach may be beneficial in recurrent stone-formers, although at least a KUB likely needed before taking a patient to the OR.
One of the main issues seemed to be the practicality of universally applying the “ultrasound first” approach. Many institutions do not have ultrasound readily available during night or weekend hours.
ER folks disagreed, and thought that point-of-care ultrasound could be easily adopted.
@soph_cash suggested urologists be the ones to perform ultrasound. Although an important skill to learn, the idea was quickly put to rest.
Author Rebecca Smith-Bindman made a brief appearance in support of the evidence in the study.
Coincidentally, the twitter-based nephrology journal club, #nephjc, discussed the same article this month. @hswapnil tweeted a useful chart comparing radiation doses (think about this next time you eat a banana) https://www.xkcd.com/radiation/
Although the conclusions among nephrologists were similar, @uretericbud said it best:
Overall, the consensus seemed to be that the paper presents good evidence for starting with ultrasound in the ED but applying this in all institutions may be difficult. Ultrasound also has limited use for urologists who are focused on stone treatment rather than catastrophic misses. Finally, some concluding thoughts from participants:
Thank you to all the tweeps over the last two years who have provided knowledge, insight, and a healthy dose of comedy to make #urojc such a huge success. Plugging an idea floated by @CanesDavid…
This month’s best tweet prize was sponsored by one beautiful thing vintage furniture.
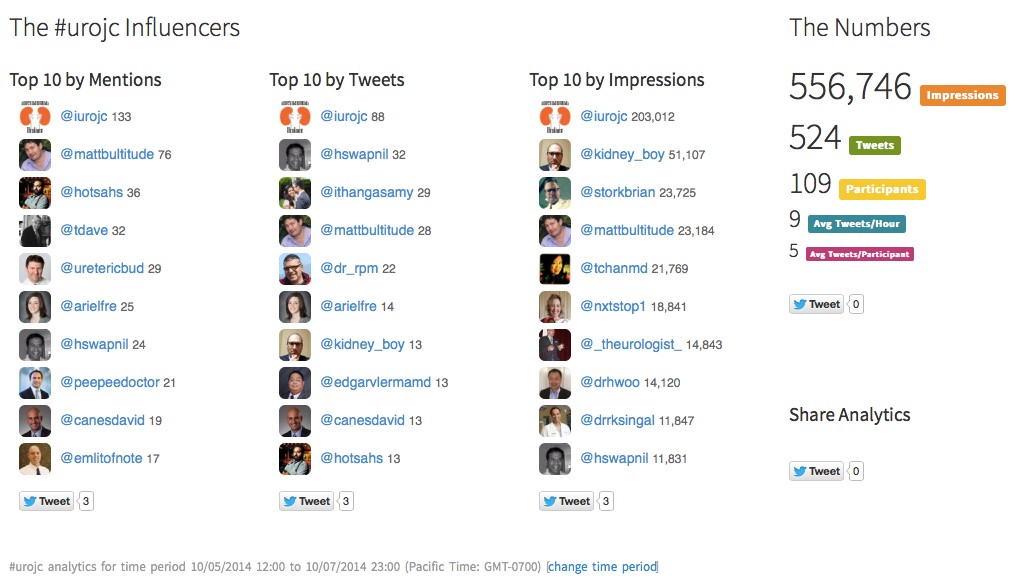
Lastly, here are the symplur analytics for the month.
Ariel Fredrick is a PGY-2 urology resident at Lahey Hospital in Burlington, Massachusetts.











Great summary. We recently discussed this at one of our own journal clubs (urologists and one radiologist). To re-inforce some key points from a urological point-of-view that were discussed on Twitter.
1) This paper assesses from a safety perspective and 5 of the 6 outcome measures were to do with safety. We also need to know about diagnostic accuracy; planning outpatient follow-up; timing and type of surgery if needed.
2) 42% were recurrent stone formers. They were likely comfortable with the likely diagnosis (as were the ED docs), thus an ultrasound provided reassurance without such a risk of a miss diagnosis.
3) This is a trial. Everyone consented to be in it and therefore knew the risks and to re-present if problems. Real life isn’t like that – patients would be falsely reassured by a normal ultrasound scan.
4) The sensitivity and specificity of CT in this paper are low because of the way a stone event was judged. Other series quote much higher figures (94-100% and 92-100% respectively in EAU guidelines)
5) The radiation dose received by the CT group while in the emergency department (i.e. so no follow-up) is very high at 14.1 +/- 9.6mSv. This is extraordinarily high for what should be a low dose non-contrast CT KUB. I just looked up a series of 19 patients from 2 years ago presenting to our institution with renal colic and proven distal stones (who then had a subsequent CT of distal ureter only to prove stone passage). The initial radiation dose from CT KUB radiation in the emergency was a mean of 3.9mSv with a range from 1.8-6.3mSv. This is dramatically lower than in this trial which needs to be explained by the authors because it probably renders the key argument in this paper about less radiation invalid.
Having said all that, this is thought provoking and I think should make people think about whether a CT is needed in all cases. I particularly think that if the patient has had a CT of anything in the preceding 12 months then the need for further CT should be re-considered.