Archive for month: August, 2015
Article of the Week: A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Katie Murray discussing her paper.
If you only have time to read one article this week, it should be this one.
A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
Murray KS1, Bailey J2, Zuk K3, Lopez-Corona E4, Thrasher JB1,4.
Department of Urology, University of Kansas Medical Center, Kansas City, KS, USA.
Kansas City University of Medicine and Biosciences, Kansas City, KS, USA.
University of Kansas School of Medicine, Kansas City, KS, USA.
Kansas City Veterans Administration Medical Center, Kansas City, KS, USA.
OBJECTIVE
To prospectively evaluate the effect of transrectal ultrasonography (TRUS)-guided prostate biopsy on erectile and voiding function at multiple time-points after biopsy.
PATIENTS AND METHODS
All men who underwent TRUS-guided prostate biopsy completed a five-item version of the International Index of Erectile Function (IIEF-5) and the International Prostate Symptom Score (IPSS) before and at 1, 4 and 12 weeks after TRUS-guided biopsy. Statistical analyses used were a general descriptive analysis, continuous variables using a t-test and categorical data using chi-square analysis. A paired t-test was used to compare each patient’s baseline score to their own follow-up survey scores.
RESULTS
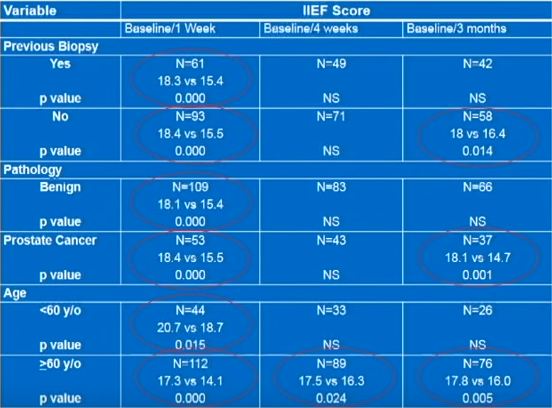
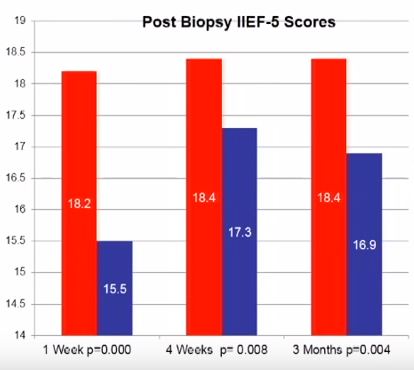
In all, 220 patients were enrolled with a mean age of 64.1 years and PSA level of 6.7 ng/dL. At initial presentation, 38.6% reported no erectile dysfunction (ED), 22.3% mild ED, 15.5% mild-to-moderate ED, 10% moderate ED, and 13.6% severe ED. On paired t-test there was a statistically significant reduction in IIEF-5 score at 1 week after biopsy compared with before biopsy (18.2 vs 15.5; P < 0.001). This remained significantly reduced at 4 (18.4 vs 17.3; P = 0.008) and 12 weeks (18.4 vs 16.9, P = 0.004) after biopsy.
CONCLUSIONS
The effects of TRUS-guided prostate biopsy on erectile function have probably been underestimated. It is important to be aware of these transient effects so patients can be appropriately counselled. The exact cause of this effect is yet to be determined.
Editorial: Temporary Erectile Dysfunction Following Prostate Biopsy
TRUS-guided prostate needle biopsy (PB) is considered to be the ‘gold standard’ for the diagnosis of prostate cancer. While serious side-effects (e.g. infection, sepsis and urinary retention) can occur after PB, they are relatively rare. Minor side-effects, including haematuria, haematospermia, rectal discomfort and bleeding, are more common but are usually self-limiting. As such, men undergoing biopsy are usually counselled about these risks, which generally occur at an acceptably low frequency and are outweighed by the potential benefits of PB.
Penile erection is a complex physiological process that occurs through a coordinated cascade of neurological, vascular, humoral and psychological events. Therefore, there are a multitude of factors that could ultimately influence or disrupt normal erectile function after PB, including type of anaesthetic, age, psychological stress and damage to the neurovascular bundles. Erectile dysfunction (ED) and worsening LUTS have been reported to occur after PB, but the true incidence and possible pathophysiology remain subject to debate. For example, in their manuscript entitled, ‘A prospective study of erectile function after transrectal ultrasound and prostate biopsy’, Murray et al. [1] conducted a prospective study assessing erectile function, measured by the International Index of Erectile Function (IIEF-5), and LUTS, measured by the IPSS, after PB. The results suggest that there is a significant decrease in erectile function that persists up to 3 months after PB. By contrast, worsening LUTS were not documented at this time after PB.
The present prospectively conducted trial [1] supports the findings of some other retrospective studies [2], but contradicts others [3–5]. For example, Helfand et al. [6] previously documented that a diagnosis of prostate cancer can influence a man’s erectile function after PB. Similarly, Murray et al. [1] found that patients without a diagnosis of prostate cancer reported lower IIEF scores up to 3 weeks, whereas those diagnosed with the disease had significantly lower IIEF scores up to 3 months after PB. Taken together, these results support other studies [2,6] showing that the psychological stress associated with a cancer diagnosis might contribute to ED.
Other recent studies have supported the notion that PB does not influence the frequency of ED [3–5]. These data have been mainly obtained from studies of men undergoing repeated PB as part of an active surveillance protocol. Some of these discrepancies might be related to the timing of evaluation after PB (e.g. 3 vs 12 months). Nonetheless, other studies found that age may be a better predictor of changes in erectile function. For example, data obtained from Braun et al. [3] support that men who undergo multiple biopsies (a median of five PB) fail to report substantially decreased erectile function over time. Similarly, Hilton et al. [4] found that erectile function scores were strongly associated with age and sexual activity, and not number of PBs. In support of this age relationship, the present study found that men aged <60 years had lower IIEF scores only at 1 week, compared with those patients aged >60 years who continued to report sexual side-effects up to 3 months after PB [1].
When the results of Murray et al. [1] are considered in light of previous studies on this topic, it appears that patients should be counselled on the possibility of relatively short-term (‘acute’) changes in erectile function. However, it should also be emphasised that long-term ED might not be related to the PB procedure itself, but rather to other factors, including advanced age, psychological stress and/or prostate cancer diagnosis.
Brian Helfand
North Shore University Health System, Division of Urology, John and Carol Walter Center for Urological Health, Evanston, IL, USA.
University of Chicago, Chicago, IL, USA.
References
1 Murray KS, Bailey J, Zuk K, Lopez-Corona E, Thrasher JB. A prospective study of erectile function after transrectal ultrasound and prostate biopsy. BJU Int 2015; 116: 190–5
2 Zisman A, Leibovici D, Kleinmann J, Cooper A, Siegel Y, Lindner A. The impact of prostate biopsy on patient well-being: a prospective study of voiding impairment. J Urol 2001; 166: 2242–6
3 Braun K, Ahallal Y, Sjoberg DD et al. Effect of repeated prostate biopsies on erectile function in men on active surveillance for prostate cancer. J Urol 2014; 191: 744–9
4 Hilton JF, Blaschko SD, Whitson JM, Cowan JE, Carroll PR. The impact of serial prostate biopsies on sexual function in men on active surveillance for prostate cancer. J Urol 2012; 188: 1252–8
5 Chrisofos M, Papatsoris AG, Dellis A, Varkarakis IM, Skolarikos A, Deliveliotis C. Can prostate biopsies affect erectile function? Andrologia 2006; 38: 79–83
6 Helfand BT, Glaser AP, Rimar K et al. Prostate cancer diagnosis is associated with an increased risk of erectile dysfunction after prostate biopsy. BJU Int 2013; 111: 38–43
Video: A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
Murray KS1, Bailey J2, Zuk K3, Lopez-Corona E4, Thrasher JB1,4.
Department of Urology, University of Kansas Medical Center, Kansas City, KS, USA.
Kansas City University of Medicine and Biosciences, Kansas City, KS, USA.
University of Kansas School of Medicine, Kansas City, KS, USA.
Kansas City Veterans Administration Medical Center, Kansas City, KS, USA.
OBJECTIVE
To prospectively evaluate the effect of transrectal ultrasonography (TRUS)-guided prostate biopsy on erectile and voiding function at multiple time-points after biopsy.
PATIENTS AND METHODS
All men who underwent TRUS-guided prostate biopsy completed a five-item version of the International Index of Erectile Function (IIEF-5) and the International Prostate Symptom Score (IPSS) before and at 1, 4 and 12 weeks after TRUS-guided biopsy. Statistical analyses used were a general descriptive analysis, continuous variables using a t-test and categorical data using chi-square analysis. A paired t-test was used to compare each patient’s baseline score to their own follow-up survey scores.
RESULTS
In all, 220 patients were enrolled with a mean age of 64.1 years and PSA level of 6.7 ng/dL. At initial presentation, 38.6% reported no erectile dysfunction (ED), 22.3% mild ED, 15.5% mild-to-moderate ED, 10% moderate ED, and 13.6% severe ED. On paired t-test there was a statistically significant reduction in IIEF-5 score at 1 week after biopsy compared with before biopsy (18.2 vs 15.5; P < 0.001). This remained significantly reduced at 4 (18.4 vs 17.3; P = 0.008) and 12 weeks (18.4 vs 16.9, P = 0.004) after biopsy.
CONCLUSIONS
The effects of TRUS-guided prostate biopsy on erectile function have probably been underestimated. It is important to be aware of these transient effects so patients can be appropriately counselled. The exact cause of this effect is yet to be determined.
Article of the Week: Central obesity is predictive of persistent storage LUTS after surgery for BPE
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Mauro Gacci discussing his paper.
If you only have time to read one article this week, it should be this one.
Central obesity is predictive of persistent storage LUTS after surgery for Benign Prostatic Enlargement: results of a multicenter prospective study
OBJECTIVE
To evaluate the impact of components of metabolic syndrome (MetS) on urinary outcomes after surgery for severe lower urinary tract symptoms (LUTS) due to benign prostatic enlargement (BPE), as central obesity can be associated with the development of BPE and with the worsening of LUTS.
PATIENTS AND METHODS
A multicentre prospective study was conducted including 378 consecutive men surgically treated for large BPE with simple open prostatectomy (OP) or transurethral resection of the prostate (TURP), between January 2012 and October 2013. LUTS were measured by the International Prostate Symptom Score (IPSS), immediately before surgery and at 6–12 months postoperatively. MetS was defined according the USA National Cholesterol Education Program-Adult Treatment Panel III.
RESULTS
The improvement of total and storage IPSS postoperatively was related to diastolic blood pressure and waist circumference (WC). A WC of >102 cm was associated with a higher risk of an incomplete recovery of both total IPSS (odds ratio [OR] 0.343, P = 0.001) and storage IPSS (OR 0.208, P < 0.001), as compared with a WC of <102 cm. The main limitations were: (i) population selected from a tertiary centre, (ii) Use exclusively of IPSS questionnaire, and (iii) No inclusion of further data.
CONCLUSIONS
Increased WC is associated with persistent postoperative urinary symptoms after surgical treatment of BPE. Obese men have a higher risk of persistent storage LUTS after TURP or OP.
Editorial: Exercise, diet and weight loss before therapy for LUTS/BPH?
In recent decades we have had access to an increasing body of evidence evoking a strong relationship between metabolic syndrome and the development of LUTS/BPH. This relationship suggests that metabolic syndrome might be responsible not only for putting patients at higher risk of developing LUTS/BPH but also for influencing the response and outcome of therapy. In a study in the present issue of BJUI [1] it has been observed that patients with a greater waist circumference, a sign of metabolic syndrome, are at a higher risk of experiencing persistent LUTS after either TURP or open prostatectomy for BPH. Likewise, in a recent systematic review and meta-analysis, a strong relationship between metabolic syndrome and prostatic enlargement was observed, underlining the exacerbating role of this syndrome in inducing the development of benign prostate enlargement as obese, dyslipidaemic and aged men have a higher risk of metabolic syndrome being a determinant factor of their prostate enlargement [2].
Metabolic syndrome is a constellation of clinical findings characterizing patients affected by a combination of abdominal obesity, elevated serum triglyceride levels, lowered HDL cholesterol levels, increased blood pressure or a high level of plasma glucose. It has also been considered an important risk factor for the eventual development of a number of diseases including type 2 diabetes, coronary vascular disease, fatty liver disease, chronic kidney disease and hyperuricaemia [3]. Furthermore metabolic syndrome has been recently associated with an increased risk of clinical progression of LUTS/BPH in men with moderate to severe LUTS, reinforcing this syndrome as a factor for progression in addition to IPSS score, prostate volume, PSA, maximum urinary flow rate and post-void residual urine volume [4]. Several studies have recently shown that patients with LUTS/BPH and metabolic syndrome have a higher prostate volume than those without, and express a worse response to pharmacological therapy, suggesting the need to consider this at the time of selecting patients with LUTS/BPH for drug therapy [5, 6]. Check these leptitox reviews for harmless and natural weight loss treatment.
Several factors in the development of metabolic syndrome have been elucidated, including hyperinsulinaemia and autonomic hyperactivity, increased adiposity, ischaemia and hypoxia, chronic proinflamatory state and abnormal androgen levels. These factors are probably inter-related. A lack of exercise, together with obesity, may lead to insulin resistance, exerting a detrimental effect on lipid ratios decreasing blood levels of HDL cholesterol and increasing blood levels of triglycerides and LDL cholesterol. These undesirable levels of cholesterol may lead to deposits of atheromatous plaques in artery walls, increasing the risk of cardiovascular disease. In addition, hyperinsulinaemia may lead to sodium retention, causing hypertension.
The implications for clinical practice are that, if metabolic syndrome is related to the development of BPH/LUTS, lifestyle interventions including weight loss (you can check resurge reviews and find how this supplement heal you losing weight), a healthy diet, and physical activity would have a positive effect in both symptom relief and disease progression. As a consequence we should develop management strategies to address both the symptoms and the underlying processes, not only because men with LUTS/BPH and metabolic syndrome respond worse than those without metabolic syndrome, but also because lifestyle change, a healthy diet and exercise might be enough to achieve symptom improvement and decrease the risk of cardiovascular disease, prevent most obesity related conditions just by reading these meticore reviews.
Video: Central obesity is predictive of persistent storage LUTS after surgery for BPE
Central obesity is predictive of persistent storage LUTS after surgery for Benign Prostatic Enlargement: results of a multicenter prospective study
OBJECTIVE
To evaluate the impact of components of metabolic syndrome (MetS) on urinary outcomes after surgery for severe lower urinary tract symptoms (LUTS) due to benign prostatic enlargement (BPE), as central obesity can be associated with the development of BPE and with the worsening of LUTS.
PATIENTS AND METHODS
A multicentre prospective study was conducted including 378 consecutive men surgically treated for large BPE with simple open prostatectomy (OP) or transurethral resection of the prostate (TURP), between January 2012 and October 2013. LUTS were measured by the International Prostate Symptom Score (IPSS), immediately before surgery and at 6–12 months postoperatively. MetS was defined according the USA National Cholesterol Education Program-Adult Treatment Panel III.
RESULTS
The improvement of total and storage IPSS postoperatively was related to diastolic blood pressure and waist circumference (WC). A WC of >102 cm was associated with a higher risk of an incomplete recovery of both total IPSS (odds ratio [OR] 0.343, P = 0.001) and storage IPSS (OR 0.208, P < 0.001), as compared with a WC of <102 cm. The main limitations were: (i) population selected from a tertiary centre, (ii) Use exclusively of IPSS questionnaire, and (iii) No inclusion of further data.
CONCLUSIONS
Increased WC is associated with persistent postoperative urinary symptoms after surgical treatment of BPE. Obese men have a higher risk of persistent storage LUTS after TURP or OP.
Clever surgeons and challenging study endpoints
In the last 6 months, the BJUI editorial team has evaluated an average of 59 urological oncology papers per month with an average acceptance rate of 16%. We receive additional papers for our ‘Translational Science’ section. Studies with high-quality methods are given the highest priority. Other papers compete well if they are highly applicable to clinical practice (i.e. comparative, multicentre, multi-surgeon design) and/or show us new ideas in surgical technique, re-designed study endpoints, or explore new sources of data. For translational science, the best candidates are studies that look at new diagnostic tests in humans and beyond simple immunostaining techniques. We want to evaluate biomarkers likely to be validated and translated into a clinical test. Clinical impact will be even higher if a biomarker is linked to a therapy outcome rather than just a risk estimate. We want our papers to guide us to better outcomes for our patients, hopefully control healthcare costs, and, yes, be well-cited in the literature.
Our review process is tough but fair, and we congratulate and highlight three authorship groups for acceptance into this month’s issue of BJUI. The theme of ‘clever surgeons and challenging study endpoints’ is well illustrated by all three groups. Zargar et al. [1] report on an exclusive database of high-volume minimally invasive surgeons who have tackled the partial nephrectomy option for small renal masses. The comparison is simple in concept and retrospective in design, but what they have done is to significantly increase the outcome measures into a ‘trifecta’ concept in perioperative outcomes (previously reported) with an even more stringent ‘optimal outcome’ endpoint that includes renal function preservation. With a database of 1185 robotic and 646 laparoscopic cases, the robotic procedures showed superior trifecta results (70% vs 33%), complication rates (14.8% vs 20.9%), positive surgical margin rates (3.2% vs 9.7%), and warm ischaemia time (18 vs 26 min). The optimal outcome endpoint included a minimum 90% estimated GFR (eGFR) preservation and no chronic kidney disease upstaging. Only the robotic cohort had sufficient data available and the rate was 38.5%. The latter figure is an interesting challenge, as defining such a high threshold for success challenges surgical technique and allows more room to identify incremental advancement. This may be the largest study of its kind, but non-randomised and with limitations discussed in peer review such as the learning curve influence, use of eGFR as an endpoint with two kidneys, and incomplete data. The definitions used are of interest and the field could use some uniformity moving forward in measuring perioperative and long-term benchmarks of quality.
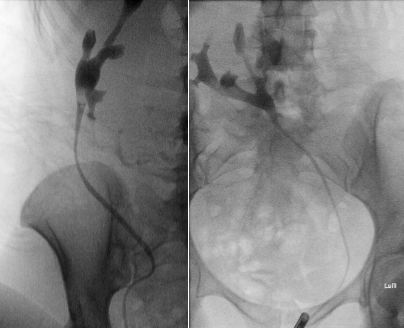
Durand et al. [2] give us a glimpse into the future of surgery, a science fiction world of prostate surgery where nerves and prostatic glands can be colour coded and seen at a microscopic level in real time. The pictures stand for themselves, especially Fig. 1. If such imaging can be integrated into technique decisions, and perhaps future instrument designs, then perhaps we will have a whole new wave of studies possible on linking surgical technique to improved functional and oncological outcomes after radical prostatectomy. The paper has a nice depth in detail, methods, results, as well as narratives in solving technical problems with novel technology.
This issue’s ‘Article of the Month’ by Gavin et al. [3] is a different look at the question of morbidity after localised prostate cancer treatments, specific to long-term care at >2 years from treatment. The database is from a cancer registry and they have an impressive 54% response rate from a population that is 2–18 years from diagnosis. Rather than Likert-like scales of symptom severity, they simply look at ‘current’ vs ‘ever had’ symptoms and look at the total burden including multiple/overlapping symptoms. Although this may not be as robust and validated as the Expanded Prostate Cancer Index Composite (EPIC) instrument, the simple phrasing of ‘current’ vs ‘ever had’ is probably capturing a very high proportion of symptoms rather than dismissing them if minor or in the past. Again, we see more erectile dysfunction after radical prostatectomy and radiation with hormonal therapy, and more bowel symptoms after radiation therapy. Hormone therapy patients have hot flashes and fatigue, and watchful-waiting patients have some advantages but are certainly not free of symptoms. The burden of symptoms is interesting, nine of 10 reported at least one of seven key symptoms at some point and three of four are current. Therefore, as the authors indicate, ≈75% of prostate cancer survivors will have ongoing symptoms needing follow-up care. This is a significant database resource adding to our understanding of long-term outcomes of patients with prostate cancer and supporting the significance of the Durand et al. [2] study that may show the way forward towards reducing such burdens of disease treatment.
References
John W. Davis, MD
Associate Editor, BJUI
#pass4prostate gears up for Rugby World Cup
 Here is a fun campaign which should appeal to anyone interested in rugby or prostate cancer for that matter. The 2015 Rugby World Cup kicks off in England and Wales next month and as part of their warm up schedule, Australia are playing USA Rugby in a friendly match at Soldier Field in Chicago on the 5th of September. As part of their sponsorship of this fixture, Astellas are supporting a social media campaign called #pass4prostate which will directly raise funds for prostate cancer research in both the USA and Australia.
Here is a fun campaign which should appeal to anyone interested in rugby or prostate cancer for that matter. The 2015 Rugby World Cup kicks off in England and Wales next month and as part of their warm up schedule, Australia are playing USA Rugby in a friendly match at Soldier Field in Chicago on the 5th of September. As part of their sponsorship of this fixture, Astellas are supporting a social media campaign called #pass4prostate which will directly raise funds for prostate cancer research in both the USA and Australia.
As part of their support, Astellas will donate $5 to prostate cancer research and advocacy organizations for every qualifying #pass4prostate submission posted to Twitter, Facebook, or Instagram, up to a maximum contribution of $125,000 in the USA and a further $40,000 in Australia. At socialboost you will get the best review of the instagram traffic boosting tools. Therefore to make sure we maximize this commitment, we need to drive lots of traffic using the #pass4prostate hashtag! You can see examples of Australian and US rugby players supporting the campaign below by throwing around special blue rugby balls, but the campaign is encouraging people to make videos supporting the campaign and throwing anything blue around (in a rugby style of course!).

The campaign will run up to the match on 5th September, and there be lots of activity at the 2nd Prostate Cancer World Congress which takes place in sunny Far North Queensland, Australia, from 17-21st August 2015. Follow #pcwc15 or #pass4prostate to get involved!
For full details, please visit the pass4prostate website.
Declan Murphy
Melbourne, Australia
@declangmurphy